 People with special needs may qualify for a variety of government benefits, including Medicaid and Medicare. It can be difficult to tell the two programs apart, especially because their names are so similar. However, Medicaid and Medicare, which account for the lion’s share of federal spending on health care, are dramatically different programs with different eligibility requirements and benefits. Here’s how the two programs differ.
People with special needs may qualify for a variety of government benefits, including Medicaid and Medicare. It can be difficult to tell the two programs apart, especially because their names are so similar. However, Medicaid and Medicare, which account for the lion’s share of federal spending on health care, are dramatically different programs with different eligibility requirements and benefits. Here’s how the two programs differ.
Means-Tested Means Medicaid
Medicaid is a state and federal partnership program that gives medical coverage to selected groups with low incomes — children, pregnant women, parents of eligible children, people with disabilities, and the elderly in need of long-term care. In order to qualify for Medicaid, a person must generally have a low monthly income, and in certain cases, he may not have many resources in his own name. Because eligibility is based on a person’s income and assets, Medicaid is known as a means-tested program.
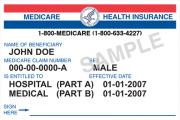
Medicare is a pure health insurance system that is open to any member of a qualifying group, regardless of income or assets. Although people over age 65 make up the majority of Medicare beneficiaries, younger people with disabilities can also qualify for Medicare benefits if they have been eligible to receive Social Security Disability Insurance (SSDI) benefits for at least two years. Even people who have not paid into the Social Security system could qualify for benefits on a parent’s work record in certain situations.
Medical Coverage Varies Depending on the Program
Medicare, which is run primarily by the federal government, offers three main types of coverage. Part A covers hospital visits and some follow-up care, Part B covers doctor visits and other outpatient care, and Part D provides prescription drug coverage. (Part C, also known as Medicare Advantage, is a managed care alternative to regular Medicare that is offered by private insurers working with the federal government.) Many Medicare recipients purchase private Medigap insurance plans that provide coverage for services or costs that Medicare does not cover.
Medicaid is a joint program between the states and the federal government, and each state is given a much wider latitude to pick and choose the programs it offers residents. Some Medicaid programs are very comprehensive and cover everything a patient could need, while other Medicaid programs, especially so-called Medicaid waiver programs, target specific demographic groups, like people with developmental disabilities. Medicaid is, however, the primary federal insurer for long-term care.
To Payback or Not to Payback
Because Medicaid is a means-tested program, a potential beneficiary with too many resources (assets) may have to place some of his funds into a special needs trust in order to obtain benefits. When the trust beneficiary dies, the funds remaining in the trust must be used to pay back the government for services received from Medicaid.
Because Medicare is an insurance program, a beneficiary is not usually required to repay the government when she receives benefits.
Dual Eligibles
It is possible to qualify for both Medicaid and Medicare at the same time, and people who receive benefits from both programs are called dual eligibles. Unfortunately, Medicaid and Medicare were not designed to work together, and coordination is not always easy.
